ABOUT US
QUALITY & SAFETY
St. Louise Regional Hospital strives to provide the safest and highest quality care to our patients, their families, and our community in a manner consistent with our values. Our care plans and processes are built on evidence-based practices, and we hold ourselves to the highest standards.
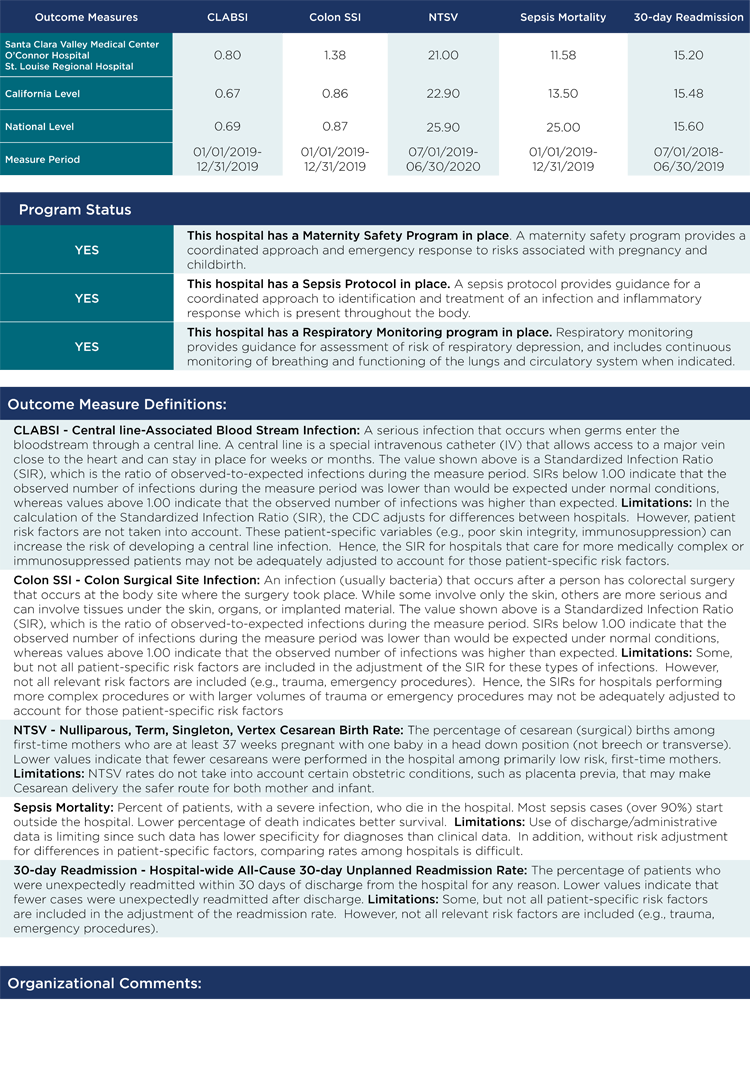
We seek to provide care that is safe, patient centered, effective, timely, efficient, and equitable. We measure our performance through a number of clinical process and outcome indicators and benchmark our performance against top performing medical centers within California and across the nation.
Dedicated to achieving excellent quality outcomes and building a culture of patient safety, St. Louise Regional Hospital has partnered with the Center for Medicare and Medicaid Services (CMS) and Premier in the Partnership for Patients Initiative to improve the quality, safety and affordability of health care for all Americans.
MEDICARE AND MEDICAID SERVICES
St. Louise Regional Hospital has been acknowledged by CMS through the Medicare’s Value Based Purchasing Program received for its performance in evidence-based care (Core Measures). These measures include best practice in the care of Acute Myocardial Infarction (heart attacks), Heart Failure, Community Acquired Pneumonia, Surgical Care, Immunizations, Perinatal Care, Sepsis Care, Stroke Care and Prevention of Thromboembolisms (blood clots).
We are committed to keeping our patients safe and protecting them from harm. We have adopted the Joint Commission’s National Patient Safety Goals and have implemented practices throughout the medical center and clinics to support patient safety. St. Louise is a Medicare provider, and is fully accredited by the Joint Commission. The hospital has also achieved Joint Commission’s Advanced Certification as a Primary Stroke Center.
TRANSPARENCY
We report our clinical care and patient experience performance data publicly through several venues: the Centers for Medicare and Medicaid (CMS), the Joint Commission and the California Hospital Compare.
The Joint Commission Public Notice Regarding Safety & Quality of Care
The Joint Commission periodically conducts an accreditation survey of St. Louise Regional Hospital. The purpose of the survey is to evaluate the organization’s compliance with nationally established Joint Commission standards. The survey results are used to determine whether — and the conditions under which — accreditation should be awarded to Saint Louise Regional Hospital.
The Joint Commission’s standards deal with organization and safety quality-of-care issues and the safety of the environment in which care is provided.
As a patient, family member, community representative or associate of St. Louise Regional Hospital, you have the right to notify The Joint Commission regarding any concern about the quality of care provided, safety of care provided, or safety of the environment in which care is provided. Anyone believing that he or she has pertinent and valid information about such matters should notify The Joint Commission.
Division of Accreditation Operations
Office of Quality Monitoring
Joint Commission on Accreditation of Healthcare Organizations
One Renaissance Boulevard
Oakbrook Terrace, IL 60181
Phone 1 (800) 994-6610
Fax 1 (630) 792-5636
Email [email protected]
This notice is posted in accordance with the Joint Commission’s requirements and may not be removed.
QUALITY TRANSPARENCY DASHBOARD